|
|
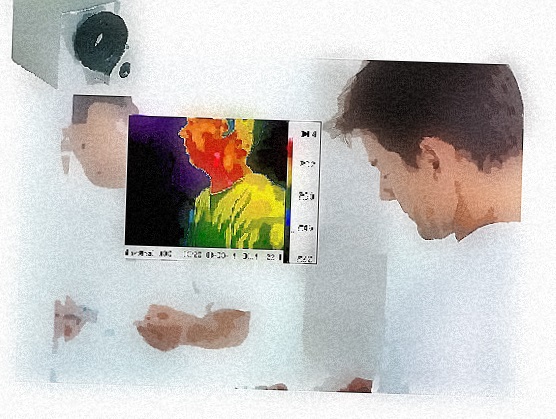
Advanced Thermal Imaging in Health Care An efficient approach to assist the physical exam by G.J. Rockley & M.G. Rockley, Ph.D. G.J. Rockley is Director of Operations for Teletherm Infrared. M.G. Rockley, Ph.D. is Director of Research & Development and is a specialist in remote infrared passive sensing who also holds 12 U.S. Patents in related technologies. ________________________________________________ One day in the future, we’ll
look into the bathroom mirror and beside our
reflection, we’ll also view a colorized
thermal image, which will enable a quick
assessment of our health condition.
Temperature designations will appear on
command for each physical area with
evaluations. This is not too far away,
especially with the rate of infrared imaging
camera development, and computer
processing. The technology is
certainly appropriate for our current need
to pursue devices that assist our lives and
can be beneficial towards the direction we
take with our physical needs.
Measuring temperature differences was fundamentally important to the Greek physician, Hippocrates. The amount of difference was noteworthy for him. He would place mud-soaked cloths across the thorax of his patients, and where the mud dried first, it was an indicator of a disease process, or location of a disorder. This early understanding gave way to evaluating human body thermoregulation, and how human body surface temperatures relate to underlying physical problems. This is a field now referred to variously as thermology, medical tele-thermography, and medical thermal imaging. The study of heat Living organisms generate heat. This heat radiated from the surface can be detected through the use of an infrared imaging camera. It maps the temperature distribution over a region of the body very quickly. The science of thermology or thermotics is the study of heat. Each anatomical region has a distinctive thermal pattern and associated thermal differences due to local variations in vascularity and surface circulatory efficiency. Typically, a baseline thermal profile is established for a patient, and then monitored over time. Thermal images are, in many ways, a first line of visualization of underlying functional abnormalities. When there is a challenge placed on the human system, such as trauma, sudden thermal shock from heat or cold, or from an internal disorder, there will be an alteration to the thermal patterns associated with an area. This is from a change to the microcirculation near the surface of the skin. There is an observable alteration in the natural process of thermoregulation, whereby the body exchanges heat through the surface of the skin with the environment, and maintains core temperature. The computer systems attached to the infrared cameras record these thermal changes, digitally, and allow for subsequent post-processing analysis and interpretation. Human body as efficient radiator Since the surface of the human body is a highly efficient radiator (emissivities ranging from ca. 0.94 to 0.99), and since that surface is not at absolute zero Kelvins, the surface radiates light as a black body radiator. For the purposes of this discussion, it may be noted that the 50% intensity points of this emission band are located across the 8-12 micron wavelength range, often referred to as the long wave infrared band (by physicists) or the mid-IR (by chemists). The wavelength peak of the emission shifts to shorter wavelength as the surface increases in temperature. However, the integrated intensity across this band is very closely approximated by a linear function of the surface temperature over small temperature ranges. Thus, by using a bandpass filter on the imaging optics to restrict the imaging to the 8-12 micron range, and integrating the received intensity across that band at each point in the plane of the source (the surface of the human subject), a temperature map of the surface may be inferred. In short, by measuring the infrared emission intensity from the skin, a thermal map of temperature distribution of that surface may be obtained through the remote non-contact sensing of the infrared imager. The thermal map will vary according to the physiological challenges placed on the body. Subsequent analysis of this image provides an ideal way to assess a patient’s physiological condition as a result of medications, surgeries, and therapies. Any changes to the neuro-vascular system will result in either increased or decreased temperature at the surface of the body, as the brain is constantly sending signals to the various areas. These, in turn, are characterized by increased or decreased infrared emission intensity on the thermal image. History of Infrared In the year 1800, the infrared portion of the light spectrum was discovered by Sir William Herschel, in Bath, England. He was the English Court Astronomer, and noted for his discovery of the planet Uranus. His findings were done through measuring the temperatures beyond the visible red using a crystal mounted on a window to throw a color spectrum onto a table where thermometers were placed. The maximum temperature was recorded beyond the visible red. As a result of this work, it was his son, John, who created the first thermal image, which was an evaporograph, based on alcohol and carbon. Now in the 21st Century, the method of evaluating subtle temperature variations is valuable to modern astrophysicists, who are currently analyzing deep space, where they’re seeing new worlds with high powered infrared telescopes. The advances in the space program and with military applications has led to the use of small, compact infrared cameras with high resolution and sensitivity that can fit in the palm of the hand. They’re being used today by physicians in all specialties around the world, with their desire to view the subtle heat variations on the human body, efficiently, and non-invasively. Medical Use The F.D.A. in the United States recognizes thermographic measurement for the adjunctive evaluation of musculoskeletal, peripheral vascular, cerebral vascular, breast and thyroid, inflammatory and neoplastic conditions. Advocates of the technology believe this imaging method is a way to identify health problems at a very early stage. In simplest form, medical thermal imaging is best considered to be the third leg of the diagnostic imaging triad of structure, chemistry and function. Conventional and cross sectional X-ray imaging provides structural information on the subject. Magnetic resonance imaging (MRI) provides both a structural and a localized, but 3-dimensional chemical volume imaging element (voxel) of the body. The third leg of this imaging triad is Infrared Thermal Imaging which provides a referred functional map of the body. Structure and function, abnormalities associated with these, trauma, and acute/chronic conditions will all change the underlying circulatory activity. This is directly referenced by the nearby surface temperature. The mapping of dermatomes (areas of skin supplied by a specific spinal nerve) plays a major role in thermal imaging and its ability to measure neural dysfunction. As an example, low back impairment can be evidenced by significant temperature differences from one extremity to the other. The plantar surface of the feet is a good measure of this. A supportive imaging method As thermal imaging is adjunctive, it is not considered solely diagnostic and in relation to X-rays, it can complement the structural information provided by the X-ray, leading to a more thorough examination. It can also help with the other imaging methods by enabling a more precise set of views, rather than a generalized approach, thereby reducing exposure. At the Department of Neurosurgery in Yongdong Hospital, Seoul, Korea, “the areas of thermal change in cervical disc herniation can be helpful in diagnosing the level of disc protrusion and in detecting the symptomatic level in multiple cervical disc herniation patients.”1 Some patients are not candidates for MRI, for example, and therefore, thermal imaging is a low cost initial step, especially when symptoms are non-specific or multi-faceted. Its use in brain surgery at the University of Southern California is revolutionary where they’ve determined the potential for thermal imaging to locate the margins of primary and metastatic brain tumors.2 Earlier work, published in 2002 by Mayo Clinic, demonstrated, intraoperatively, that infrared imaging “exhibited the distinct thermal footprints of 14 of 16 brain tumors.” It provided “real-time assessment of cerebral vessel patency and cerebral perfusion.”3 Time, volume of patients, and previously undiagnosed conditions all contribute to making the initial patient examination challenging for the dedicated physician. Therefore, thermal imaging with an infrared camera system can be an efficient and highly objective way to get valuable physiological data that can make a difference. It is absolutely non-contact, with no radiation or penetrating forces being sent into the body. The thermal imaging test facilitates early diagnosis and successful treatment plans. It can preclude the necessity for performing more invasive tests that could be painful, stressful, or even hazardous, and even avoid those procedures that might prolong recovery. Thermal imaging also helps to verify a patient’s progress through therapy and rehabilitation. Repeated passive infrared images can be sequentially compared. It can help document whether novel and unusual treatments and therapies have benefit and show progress for the patient. The test can also indicate whether change is temporary or more permanent. |
 Noteworthy Clinical
Studies
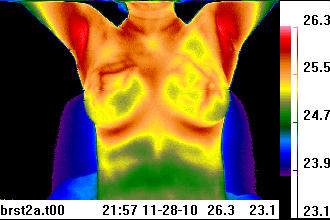
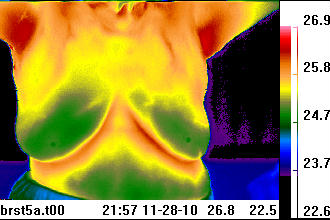
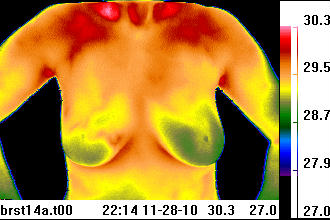
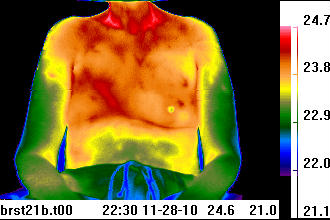
The scanning of children and expectant mothers are excellent examples of the value with thermal imaging. At the Department of Pediatric Surgery, Medical University of Graz, Austria, "IRT (infrared thermal imaging) was found to be an excellent noninvasive tool in the follow-up of hemangiomas, vascular malformations and digit amputations related to reimplantation, burns as well as skin and vascular growth after biomaterial implants in newborns with gastroschisis and giant omphaloceles. In the emergency room, it was a valuable tool for rapid diagnosis of extremity thrombosis, varicoceles, inflammation, abscesses, gangrene and wound infections."4 With the expectant mother, the thermal image poses no risk to the baby, especially if the mother is complaining of other health conditions or suffers from low back problems. The University of Michigan, Department of Ob-Gyn in the mid 1990’s conducted a study for using infrared thermal imaging for the evaluation of preterm rupture of the fetal membranes. It showed potential for being a sensitive clinical indicator for chorioamniotic infection.5 It’s an ideal test to provide the physician with one more piece of information which can be used to better treat the mother. Thermal imaging has applications in breast oncology, integrative medicine, plastic surgery, chiropractic, dentistry, orthopedics, acupuncture, occupational medicine, pain management, vascular medicine, cardiology and veterinary medicine. Novel uses now being developed include sleep studies and stress research. One of the more recognized applications has been for breast examinations. Of some note is the recognition that invasive breast cancer in its early stages exhibits little structural abnormality (thus escaping routine structural imaging recognition). Rather, it is detected often by a skilled technician using their hands to assess the side to side breast temperature differential. This is somewhat less effective than the use of a thermal imaging camera with a temperature resolution on the order of 50 mK (milli Kelvins). Unfortunately, a poorly conducted U.S. National Cancer Institute study in the late 1970’s with untrained physicians and cumbersome early thermal cameras tainted the prospects of the test being used in this regard. Not until the late 1990’s, with the improved efficiency and sensitivity of the infrared imaging cameras, did the viability of thermal imaging for breast evaluations become more widely recognized. Most recently, a report from New York Presbyterian Hospital, Cornell, NY, found infrared thermal imaging to be “a valuable adjunct to mammography and ultrasound, especially in women with dense breast parenchyma."6 The non-radiating aspect is certainly attractive, and the level of ease for conducting the test, with regular risk-free follow-up at low cost, is also appealing. ____________________________________ Online Educational Programs Which image is most symmetrical, thermally?
Send us your choice for which is the most symmetrical image above. Click here to enter ____________________________________ The procedure With the latest technology, now incorporating wireless control, remote viewing capabilities and capture of thermal images are easily achieved. This enables the subject to be scanned in a typical 4x6 foot area, in a complete privacy booth. The region of the body being scanned should be exposed, with the clothing and jewelry removed. Things to consider would be the size of the area being viewed with the imager, time of the scan, female versus male subjects, health condition of the subject, nature and longevity of underlying physiological abnormalities of the subject, positioning of the subject, and comfort of the subject. The design of the camera and the software all contribute to the ease of use and elimination of technician error in the process. For medical applications, it’s helpful to have a controlled environment and established procedures for conducting the test. The imager is typically placed at a distance of 36-48 inches from the subject, with a neutral background located a few inches behind the patient. The patient should not lean against the background wall or screen. Each of these variables must be controlled in order to make the most reliable inferences regarding the efficacy of a particular course of treatment or correlating with the complete diagnostic workup. Understanding the thermal image colors The intensity of the infrared light emitted by the surface of the subject is converted by computer algorithms into a ‘false color’ palette. Flexibility in palette use is quite important. This is simply because there is some interpretation of the image involved, and the human eye functions by logarithmic color contrast analysis. Thus, the heat map of the subject becomes a colored image. Typically, blue colors represent cooler regions while red colors represent hotter regions, but there are arguments for white/black and black/white images, and an amazing variety of hybrid palettes for different types of images. These images show the areas on the body where there is increased or decreased circulatory activity. Bony areas will typically appear colder while regions associated with soft tissue such as under the arms will appear hot. Symmetry is the norm. Most thermal images or thermograms have a color scale appearing alongside the actual image, where temperatures for each particular color in the image are noted. The cooler colors are typically designated at the bottom of the scale, and usually in darker colors such as blues, while the hotter colors are at the top usually in the lighter shades such as the reds. The more moderate temperature value designations are in the middle, depicted in the greens and yellows on more recognizable color scales. The physician should identify the various regions in the image that are hot and/or cold and whether or not this is ‘typical’ for all patients or for the particular patient, evaluating the symmetry of the image, while also looking for anomalous localized heat spots or unusual cold spots within the image. For example, a total thermal ‘cutoff’ in the feet or hands (term for very low radiative intensity in the 8-12 micron range) indicates that these extremities are very cold, suggesting additional testing for conditions such as Raynaud’s or long term sympathetically maintained pain conditions, or chronic injuries. Low cost Due to the digital nature of thermal imaging, the actual cost of operation is minimal. It primarily rests on technician fees. Cost of equipment has also come down substantially, with thermal imagers starting at less than ten thousand dollars US. However, it’s important to have an imaging system designed for clinical use and from manufacturers familiar with real world medical applications, with software that supports image post-processing. With the continuing sophistication of thermal imaging instruments, computing power, combined with documented case research examples, many more benefits will emerge, whereby automated analysis will enable physicians to be highly informed with regard to case management. The volume of work being conducted throughout the world, on a continuing basis with thermal imaging, is significant. It contributes to this diagnostic and monitoring option being of paramount importance to the modern clinical practice of the future. The ancient Egyptians used the scanning ability of their hands with their brain acting as a computer. They understood that temperature rose and fell over time, and localized in a specific wound or was generalized over the entire body.7 We now have these advanced tools with infrared thermal imaging and tablet computers to assist us instantaneously, and in an extremely visual and non-intrusive way. ___________________________________ 1 Yonsei Med J 1999 Oct;40(5):401-12. Thermatomal changes in cervical disc herniations. Zhang HY, Kim YS, Cho YE; Department of Neurosurgery, Yongdong Severance Hospital, Yonsei College of Medicine, Seoul, Korea. 2 Neuroimage. 2009, Mar 28. Intraoperative Thermal Imaging. USC, Department of Neurological Surgery, Keck School of Medicine, Department of Radiology. 3 J Neurosurg 2002 Dec;97(6):1460-71. Vision of the future: initial experience with intraoperative real-time high-resolution dynamic infrared imaging. Technical note. Ecker RD, Goerss SJ, Meyer FB, Cohen-Gadol AA, Britton JW, Levine JA. Department of Neurological Surgery, Mayo Clinic and Foundation, Rochester, Minnesota. 4 Eur J Pediatr. 2007 Aug 30. Infrared thermography: Experience from a decade of pediatric imaging. Department of Pediatric Surgery, Medical University of Graz, Auenbruggerplatz 34, Graz, Austria 5 Biomedical Instrumentation & Technology Nov/Dec. Application of Telethermography in the Evaluation of Preterm Premature Rupture of the Fetal Membranes. Michael Sheinberg, MD, Robert Hayashi, MD, et al. Dept. of Obstetrics & Gynecology, University of Michigan Hospitals, Antenatal Testing Unit, Ann Arbor, Michigan. 6 Am J Surg. 2008 Oct;196(4):523-6. Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer. Department of Surgery, New York Presbyterian Hospital-Cornell, New York, NY 7 Medical Thermology. Edited by Margaret Abernathy, M.D., Sumio Uematsu, M.D.. 1986. ISBN 0-9614905-0-0. P. 2 |
Email address: teletherm@thermology.com
Teletherm Infrared Systems / Research (813) 466-2795 - Tampa, Florida U.S.A.
Teletherm Infrared Systems / Research (813) 466-2795 - Tampa, Florida U.S.A.
(C)
Copyright 1999-2025Teletherm Infrared Systems /
Research, - Tampa, FL.
USA
email: teletherm@thermology.com
All rights are reserved worldwide.
(C)
Copyright 2005-2025 Teletherm color palette
designation EYESC3, EYECLOSE1, Teletherm
Infrared Systems / Research - Tampa, FL.
USA. All rights are reserved worldwide.